
Creighton Nursing & CommonSpirit to Pilot AI Prototype to Enhance Patient Care

The National Institutes of Health estimates approximately 250,000 fall-related injuries occur in U.S. hospitals annually. Risk factors for hospital falls are many—longer stays, illness-related weakness, post-operative balance troubles, the sedative effect of medications, urine incontinence, visual impairment and more—but useful solutions are few.
“Falls are just one clinical problem for which we simply don’t have an effective prevention protocol,” says Mandy Kirkpatrick, PhD, RN, FAAN, FNAP, associate dean for research and innovation at Creighton University College of Nursing.
It’s a conundrum that CommonSpirit Health aims to address with its Virtually Integrated CareSM (VIC) program by partnering with Creighton University in the design of an AI-enhanced nursing platform that assists in the prevention of falls and pressure injuries.
Mentors for nurses, immediate care for patients
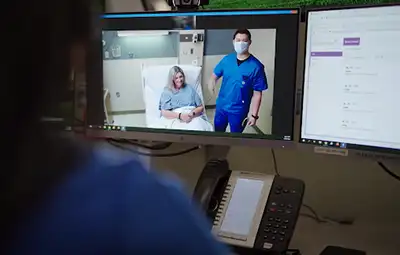
First launched in 2016 by CommonSpirit Health, VIC is the first virtual nursing model of its kind employed in progressive and acute care units. It uses advanced, all-in-one computer technology in which nurses, working remotely, interface with unit nurses and patients. They have access to patient medical records and can converse with patients and nurses on screens in hospital rooms, much like Zoom calls. Patient privacy is carefully guarded; cameras are only turned on after the virtual nurse requests communication and the patient grants permission.
Virtual nurses assist floor nurses with numerous tasks, including patient education, administrative tasks such as admissions and discharge, pain assessment and family meetings, freeing up bedside nurses to accomplish other hands-on tasks. The goal of VIC is to provide newer, less-experienced nurses with seasoned mentors who offer advice and guide plans of care.
“For the newly graduated nurse, the virtual nurse is a welcomed extra set of eyes, someone to bounce ideas off of,” says Kirkpatrick.
Anne Schoening, PhD, RN, nursing practice coordinator at CHI Health Creighton University Medical Center - Bergan Mercy, calls VIC nurses “an amazing resource” and “an invaluable addition to our bedside staff.”
“Fully integrated into the care team, they play a critical role in promoting quality and safety by performing routine checks to prevent safety events, such as falls. They’ve recently joined several of our quality improvement project teams and are identifying ways they can help us prevent hospital-acquired complications, such as pressure injuries and venous thromboembolism,” she adds.
Creighton nursing faculty and computer science faculty from the College of Arts and Sciences have collaborated with CommonSpirit Health to propose the development of AI fall prevention technology for integration into the VIC platform. In their application for grant funding, they propose using AI to monitor patient movement and warn both virtual and floor nurses when patients are at risk of falling.
Their plan involves engaging faculty, students and clinicians in training AI to better understand patient fall risk by creating simulated falls recordings so AI can then identify what movements come before patient falls. Their goal is to develop an AI prototype that detects red flag movements, sending an early alert through the VIC platform to nurses, thus preventing further injury.
The team plans to develop and test the prototype at Creighton University Medical Center-Bergan Mercy.
A successful AI-enhanced fall prevention prototype would augment existing protocols like nurse call buttons, bed alarms and nonslip socks. An ultimate measure of success would be improved patient outcomes and effectively reducing length of hospital stay and costs.
“VIC exemplifies how strategic technology implementation can empower our nursing teams. By automating administrative tasks, we're not just freeing up nurses' time; we're enabling them to focus on what matters most: delivering personalized, compassionate care,” said Julie Tuel, MSN, RN, CCRN-CMC, SCRN, CAVRN, system vice president of virtual care nursing practice transformation at CommonSpirit Health. “We are thrilled to be partnering with Creighton on this important work to continue to advance nurse-led innovations that improve patient safety outcomes.”
Creighton College of Nursing and CommonSpirit Health: A winning partnership

The American Nurses Association (ANA) has recognized the Virtually Integrated CareSM program with an ANA Enterprise Innovations Honorable Mention, which highlights, recognizes and celebrates nurse-led innovations that improve patient safety outcomes. VIC was one of seven entries honored out of 330 applicants in the award’s technology category. The honor carries a $10,000 prize.
Along with Kirkpatrick, Tuel and Schoening, Steven Fernandes, PhD, assistant professor of computer science and informatics at Creighton, completes the award-winning team.
“Through the seamless collaboration of CommonSpirit Health and Creighton University College of Nursing, we have fostered a culture of innovation and excellence. This recent award symbolizes not just our achievements, but our collective commitment to transforming nursing practice,” says Jessica Clark, DNP, RN, dean of the College of Nursing. “Yet, this is only the beginning—together, we will continue to push boundaries, ensuring every advancement leads to better care and brighter futures for those we serve.”
Kirkpatrick says they will use the award to develop fall-prevention training videos later this year, after which Creighton and CommonSpirit Health hope to advance the second stage of the program – developing patient movement protocols to prevent pressure ulcers (bed sores).
“Nursing faculty and students will conduct a cause analysis and then devise solutions individualized to the units that experience high rates of pressure ulcers,” says Kirkpatrick. Engaging students in this process empowers them to be change makers and gain confidence in their ability to identify and then remedy problems.
By engaging students in real-life issues that they will confront as practicing nurses, Creighton is preparing them to be leaders in their field, whether it is through patient advocacy, affecting policy change on the state level, serving those in most need by volunteering or conducting evidence-based research and practice, as in the case with the pressure ulcer root cause analysis.
“Just as we leverage technology to balance nurse workload and impact patient care, we can—and should—leverage partnerships and interprofessional engagement to improve outcomes for our patients,” Kirkpatrick says. “We should never accept the status quo.”




